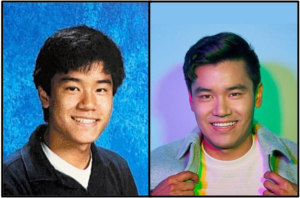
Q&A: Urologic oncologist Ashish M. Kamat discusses his COVID-19 research

F. Carter Smith
Kamat is an accomplished surgeon, professor and one of the world’s leading experts on a drug called BCG, which is normally used to treat bladder cancer.
May 4, 2020
Freshman Cameron Ederle spoke with urologic oncologist Ashish M. Kamat, parent of Rhea (’21) and Ishan (’19), to discuss how he is using his background in cancer to research the virus. Kamat is an accomplished surgeon, professor and one of the world’s leading experts on a drug called BCG, which is normally used to treat bladder cancer. When COVID-19 emerged, he joined a team to begin researching how BCG could be used to fight the virus and found some interesting results.
Could you give background on what your job before the outbreak was like?
I’m a cancer surgeon, so I do urologic oncology. I also do a lot of research, and I lead several international organizations that are related to bladder cancer work. I am a tenured professor at MD Anderson, so I have a lot of postdoc and grad students. I don’t only do surgery and research, I also teach and do training.
How do you use your background as a cancer surgeon for researching the virus?
That’s actually very interesting. One of the drugs that we use to treat bladder cancer is known as BCG, a tuberculosis vaccine that was developed in 1922. It’s been used since the 1990s to treat patients with bladder cancer because when you put it in the bladder, it stimulates the immune response and then prevents these tumors from coming back. So that’s what I do, and that’s what I am one of the world’s leading experts on.
It also has immune protective effects in the sense that when it’s given to kids and older people in places like Greece, Africa, India and other such places, it protects them from types of pneumonia and staph and skin infections. When COVID-19 came about, I reached out to my trainees around the world and had them look at data to see if countries that use this BCG vaccination had any difference in the COVID-19 response.
It turns out that yes, countries that do currently vaccinate their population with BCG had almost a ten-fold decrease in the cases of COVID-19, and almost a ten-fold decrease in deaths from COVID-19. So that led us and others to design a trial, where we’re taking this BCG and giving it as a vaccine to healthcare workers: doctors, nurses, PA’s, people who are dealing with patients, to boost their immune system and help prevent COVID-19 infection and mortality in the first place.
In the US there are a lot of rules and regulations, so we are just in the early phases. In Australia, they have already given this to 2,000 people, and in the Netherlands, they have already given it to 1,500 people.
What makes the virus so harmful?
This is a coronavirus that has never been seen in humans to date, which is why human beings don’t have any immunity to it, which is how it spreads so fast. It has properties that allow it to attack not only the respiratory system but the circulatory system and other systems within our bodies, which is why the elderly, young folks and people who already have other diseases are not able to fight off the virus.
What is your outlook on the progress of the research?
Everybody is working hard to find drugs that would work to help people that are infected, and there are some drugs that are beginning to show progress. Some people are trying to find different vaccines, one of them being the BCG vaccine, but that’s a non-specific vaccine; that’s meant to boost your immunity against anything. But they are also working to find a specific vaccine; the way development works, it usually takes about 9 months to a year, so we probably won’t have that until this time next year. The information that is coming out is slow but steady, but no big breaks yet.
When you are researching the virus, are you at risk yourself?
Yes, we are, but it’s not just because of the research. We are still taking care of patients at the hospital, so that’s the risk. But the research we are doing is not putting my team at risk other than the fact that we are in the hospital. It’s different from teams at the CDC, where they’re actually trying to study the virus itself. That research is only allowed to be done in specific virology centers, because there is a lot of talk that COVID-19 escaped from the lab in Wuhan, supposedly one of the most secure labs in the world. So clearly you cannot have this research in labs that are not certified for this kind of work.
What are the policies for cancer surgeries during the outbreak?
Cancer is not elective, so cancer patients can’t wait an “x” amount of days, because they could die. But even within the cancer paradigm, there are some cancers that you can wait a month or so, and some that cannot. So for the ones that could wait, we told the patients that it would probably be their safest option. But for the patients that cannot wait, we’re between a rock and a hard place because we know for sure that if we wait too long they’ll die of their cancer. We think that we can protect them with masks and other things, but it’s a decision between them and their doctors to take that risk. Those with aggressive cancer prefer to come and get treated.
What precautions has your hospital system (MD Anderson) taken to prevent infection?
We have been very proactive. Early on when the outbreak first started, people had to hand wash, make sure you don’t come to work with a cough, and follow social distancing. Then it got to where anyone non-essential didn’t have to come to work. Now, we were given masks, and our temperature is taken before we go into the hospital. Patients get tested, and if they test positive for COVID-19, they aren’t mixed in with the general pool.
Anything else you would like to say?
This is a serious problem, and even when all the social distancing comes down, each one of us has to be vigilant about how we expose ourselves. This is very dangerous and we don’t have anything near a definite vaccine. On the other hand, we encourage research and inquisitive minds. If you come up tomorrow with a question or idea about COVID-19 or a correlation that clicks, share it with people. Bring it up. We are seeing a lot of ideas coming in from all types of age groups that are really helping to solve this mystery.